Alzheimer's disease affects millions of people around the world, but what ultimately causes the debilitating dementia remains unknown. One controversial theory, however, holds that the disease might be the result of a virus, or multiple viruses, infecting the brain.
How does Alzheimer’s research relate to cold sores?
In the journal Neuron, researchers found that the brains of deceased people with Alzheimer's disease had higher levels of viruses than the brains of deceased people without Alzheimer's. Specifically, the Alzheimer's brains had up to twice as much of two common strains of herpes viruses than the non-Alzheimer's brains.
In one study, researchers from Umeå University in Sweden found that being a carrier of herpes simplex virus 1 (HSV1) nearly doubled a person’s risk of developing Alzheimer’s disease. In a second study, the researchers followed 3,432 people for an average of 11.3 years, and found that a reactivated herpes simplex 1 infection doubled one’s risk of developing Alzheimer’s disease. However, herpes simplex virus 1 infections are very common and once you are infected, you carry the virus for life. From time to time, the virus can become active, which can cause cold sores.
What is notable about the research is that it was well-designed. Researchers studied a large group of people, there was a long period of follow up time (two decades) and the way in which they diagnosed Alzheimer’s used methods that we can reasonably trust.
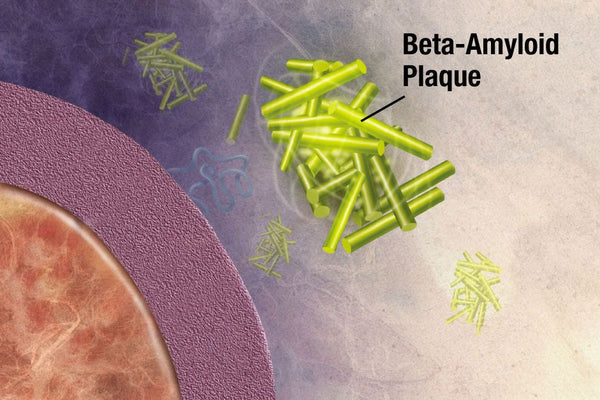
A diagnosis of Alzheimer’s disease can be made with certainty only after death, though this is changing. Neuroimaging techniques, for example, now allow visualization of amyloid plaques, which are the hallmark of Alzheimer’s.
How does the herpes virus potentially trigger or worsen Alzheimer’s?
Some researchers have proposed that herpes could, under some circumstances, lead to inflammation in the brain and changes to brain cell function. This could then potentially trigger or worsen Alzheimer's. However, herpes infection in the brain appears to be more common in people with Alzheimer's disease who have a gene called ApoE4, which is known to increase the risk of Alzheimer's. One theory behind this is ApoE4 increases the likelihood of the herpes virus moving from the body into the brain. Although there are likely to be several reasons, this might be part of the reason that people with ApoE4 are at an increased risk of Alzheimer's. Some researchers suspect ApoE4 allows more virus particles to attach themselves to brain cells, making it easier to infect them.
Having Alzheimer’s makes the brain more susceptible to infection.
The blood-brain barrier protects the brain by controlling what substances can pass from the blood into brain tissue. In Alzheimer's disease, the blood-brain barrier is damaged, particularly in the brain region affected by Alzheimer's. Once it has been weakened, bacteria, viruses, and other harmful substances can enter the brain more easily. This may explain why certain viruses, such as herpes, are more common in the brains of people with Alzheimer's.
It is worth bearing in mind that there is no strong evidence that herpes virus infection actually causes Alzheimer's disease. The increased presence of the virus in the brain may be related to changes to the immune system due to Alzheimer's disease.
What is the current HSV1 and Alzheimer’s theory?
Researchers believe that HSV1 is a major contributory factor for Alzheimer’s disease and that it enters the brains of elderly people as their immune system declines with age. It then establishes a latent (dormant) infection, from which it is reactivated by events such as stress, a reduced immune system and brain inflammation induced by infection by other microbes.
Reactivation leads to direct viral damage in infected cells and to viral-induced inflammation. Suggesting that repeated activation causes cumulative damage, leading eventually to Alzheimer’s disease in people with the ApoE4 gene.
Presumably, in ApoE4 carriers, Alzheimer’s disease develops in the brain because of greater HSV1-induced formation of toxic products, or less repair of damaged cells.
New treatment options for Alzheimer’s disease.
The data suggests that antiviral agents might be used for treating Alzheimer’s disease. The main antiviral agents, which are safe, prevent new viruses from forming, thereby limiting viral damage.
It's also been found that the anti-herpes antiviral drug, acyclovir, blocks HSV1 DNA replication, and reduces levels of beta-amyloid and tau caused by HSV1 infection of cell cultures.
It’s important to note that all studies only show an association between the herpes virus and Alzheimer’s – they don’t prove that the virus is an actual cause. The only way to prove that a microbe is a cause of a disease is to show that an occurrence of the disease is greatly reduced either by targeting the microbe with a specific anti-microbial agent or by specific vaccination against the microbe.
Excitingly, successful prevention of Alzheimer’s disease by use of specific anti-herpes agents have now been demonstrated in a large-scale population study in Taiwan. Hopefully, information in other countries will yield similar results.
Sources:
http://www.bbc.com/future/story/20181022-there-is-mounting-evidence-that-herpes-leads-to-alzheimers
https://www.livescience.com/62883-herpes-viruses-alzheimers.html
https://health.clevelandclinic.org/does-your-cold-sore-mean-youll-get-alzheimers-disease/
https://www.cell.com/neuron/fulltext/S0896-6273(18)30421-5
https://www.alz.org/alzheimers-dementia/what-is-alzheimers

